Methadone: Abolish the Clinic System, Free the Medication
Interviews with Helen Redmond, LCSW, and Sam Snodgrass, PhD
In my last post, I shared how my daughter finally got on the medication she knew she needed: methadone. While I learned about the life-saving value of this medication, she learned other things: how to get drugs in the clinic parking lot, how to work the system to make sure she could stay on the medication even though that meant lying. The methadone was wonderful for her - the clinic system was terrible.
In this issue of Ask the Experts, we return to Sam Snodgrass, PhD, who tells us about his eleven year experience with methadone clinics. We also interview Helen Redmond, Licensed Clinical Social Worker and journalist, who tells us why the methadone clinic system can and should be abolished, so that doctors can prescribe this medication directly and patients can access it at a pharmacy - just like any other medication.
Moms for All Paths: You mentioned in our previous discussion that methadone was quickly siloed into Opioid Treatment Clinics (OTC’s) or what is usually called methadone clinics. Can you say more about that?
Sam Snodgrass, PhD:
The problem with methadone is not the methadone, it’s the methadone clinics. I know that SAMHSA has released new guidelines but that’s all they are. Guidelines. If the state that you are in or your clinic doesn’t want to adhere to the new guidelines, they won’t. They can continue operating just as they have been. When I was attending a methadone clinic, you had to go to the clinic every day for the first ninety days, except Sunday when you had a take-home dose. There are some clinics that make you come in seven days a week.
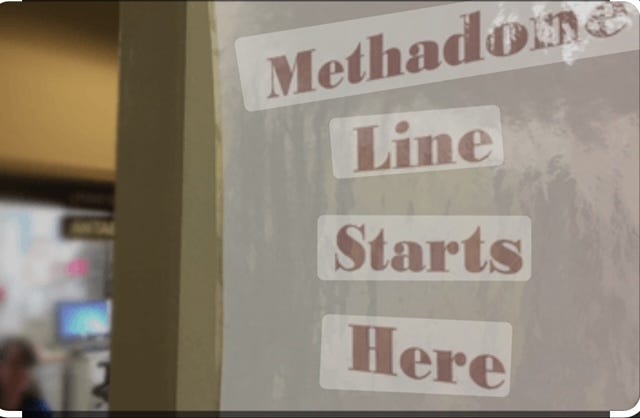
I was in a methadone clinic for eleven years. They open at 5:30 in the morning, people have to come in, get their dose, get home, get the kids ready or whatever and be at work by 8. There is, of course, a line of people waiting for the door to open and then a full waiting room, and these people are strangers. What do you think they’re going to talk about? The only thing they have in common is that they use drugs. They’re going to bitch about the clinic, rightfully so, and they’re going to talk about drugs. It’s the worst system you could imagine. You have people who are trying to do the right thing and are working to get their life back and you put them in the very situation they’re trying to get away from. You should be trying to keep people away from that kind of environment and instead they are being forced into it by the clinic system.
In the methadone clinic system, you had better get along with your counselor. They can hold your dose, get your dose reduced, and make you go to extra meetings. They have so much power over your life. The power dynamic in the methadone clinic is that the clinic has all the power and you have none. You had better go in with a smile on your face and say “Yes sir, yes ma’am,” because if you don’t, they get you in a “team meeting” where you’re in the middle of the circle and they’re telling you that you did something wrong and they’re going to take you back to coming in once a day. Or they can just kick you out of the clinic. If you can’t pay you’re out.
You’re getting there at 5:30 in the morning and you can’t dose until after you see your counselor or go to a group meeting, So they’re going to hold your dose until you get out of the meeting, then you have to get back in line to get your dose, then get to your job by 8! Methadone clinics are not that plentiful, especially in rural areas. I know people who drive an hour and a half each way. This is no way to live. It sets people up to fail.
If would be much better if we could just do it like they do in other countries where people see a physician and they can pick up their methadone at the pharmacy in their hometown, no need to drive, no required counseling. If someone wants counseling they should have access to effective counseling, but if someone doesn’t feel like they’re getting benefit from counseling, coercing them into it is just another reason to leave the clinic.
Methadone clinics also do things like call-backs, which means that they call you back for a med check and you’ve got to get there that day. You have to take off work, do whatever you have to do, and be at the clinic with your meds so they can count the bottles and look at the dates and make sure you’re taking them exactly as you're supposed to. If anything goes wrong, such as the seal on one of the bottles gets caught in the lid as they open it and the seal gets broken, they’ll say you were tampering with your medication. Then if you’ve been getting a two week supply, they’ll take you back to coming to the clinic every single day. It’s very paternalistic: the methadone clinic knows what’s right for you, knows what’s best for you. They are the parent and you are the child.
Methadone is an excellent medication, but methadone clinics are a horror show. Getting methadone out of the clinic system and back into the medical profession and regular pharmacies would go a long way toward reducing stigma and getting people this life-saving medication. There are people that won’t go to a methadone clinic because of the stigma.
Moms for All Paths: As Helen Redmond is about to describe to us, buprenorphine is easier to get. However, many people, like my daughter, do not find that buprenorphine is the right medication for them. What is the difference?
Sam Snodgrass, PhD:
Methadone is a full opioid agonist. That means that it binds the opioid receptor sites and activates them fully. Buprenorphine is a partial opioid agonist, and activates the opioid receptors only partially. They are both very effective medications.
Once you get on a stable dose of methadone, you don’t feel much of an effect: you’re just normal. This is due to tolerance. But when I was taking methadone I would feel a little bit of a bump - like a mouse with house slippers on, not much at all - about thirty to forty-five minutes after taking it. After that, I was just normal. I can’t speak for others, but for me that was important. I looked forward to taking my methadone the next morning and that’s fine. If that keeps someone in treatment, then all the better.
I’ve never taken buprenorphine but I worked with people who did for 10 years in a buprenorphine clinic. What they told me is that after the first few doses, they didn’t feel the buprenorphine. They just felt normal. Some said that after they had been taking it for a few months they would get busy and just forget to take it. When they started to feel anxious or like a cold was coming on, they would remember they hadn’t taken their buprenorphine. Many of the people, not all, but many, had medication left at the end of the month. You do not forget to take your methadone. And, again, that’s fine.
Why does one medication work better for some than the other? Methadone, being a full opioid agonist, will produce greater stability for some people than will buprenorphine. Methadone will control their craving, their starvation, for these opioids better than buprenorphine. For others, buprenorphine will work just as well as methadone. Whichever medication works best for each person is what matters. But, and this is very important, the medications work only if the person is prescribed an adequate dose. That’s not true just for methadone and buprenorphine, but for any medication. Far too often, a person is prescribed an inadequate dose of methadone or buprenorphine and is then blamed for “failing” when it’s not the person but the dose that failed. This would be unacceptable in the treatment of any other medical condition. Unfortunately, it is all too common in the treatment of opioid use disorder.
One clear advantage methadone has during this age of fentanyl is that a person can induct directly onto methadone with no problem. If the induction process with buprenorphine is not done correctly, they can be thrown into precipitated withdrawal. And, again, for many methadone is the medication that they need. It will work better for them than buprenorphine. Yet, when we have over 80,000 people dying of opioid-involved overdose deaths a year we silo methadone into these paternalistic and punitive clinics that put profits over lives. In what world is that sane?
Helen Redmond, Licensed Clinical Social Worker and Journalist:
Moms For All Paths: Thank you for joining us! Can you tell us a little bit about who you are and what you do?
Helen Redmond:
My name is Helen Redmond, and I am a Licensed Clinical Social Worker. I worked in healthcare settings for over a decade, including hospitals and clinics. I worked mostly with people who use drugs, so one of my jobs as a social worker was to help people get into drug treatment. Methadone maintenance was one of the big ones because a majority of my patients were using heroin (back when we had heroin.) So I have a good sense of the drug treatment system in the United States, and how our very dysfunctional healthcare system treats people who use drugs.
That’s the first hat I wear. The second one is as a journalist. I've been writing about drugs for over two decades. For many years now I've focused on methadone. I write extensively about methadone for a publication called Filter. The third one is filmmaker and I’ve made two documentaries about methadone: Liquid Handcuffs and Swallow This. So journalism, filmmaking and my experience on the frontlines of the healthcare crisis, working with people who use drugs, all of that informs my work.
Moms for All Paths: Sam Snodgrass described for us his experience in methadone clinics, and it seems obvious that this is a system that sets people up to fail. How did we come to be in a situation where life-saving medication is held captive in such a terrible system?
Helen Redmond:
I think it really has to do with how the United States has always seen people who use drugs as criminals, after all there is a War on Drugs, drug prohibition, and also the absolute adherence to the abstinence model. The methadone clinic system goes all the way back to a compromise that was made fifty years ago during the Nixon administration.
The research of Drs. Marie Nyswander, Vincent P. Dole and Mary Jeanne Kreek in New York City discovered that methadone stops the cravings for heroin. It allows people to feel normal, whatever normal is for each person, and then life goes on. But rather than allowing doctors to prescribe methadone and patients to pick it up in their pharmacy, the methadone clinic system was created. The Drug Enforcement Administration, the police who are carrying out prohibition, created very draconian, very carceral rules and regulations for clinics that were based on the idea that people who are addicted to drugs can’t be trusted, because they’re criminals. So they have to go to the clinic six or seven days a week, and they will be watched while taking medication, and drug tested constantly. And if you don't pass the piss test, you get kicked out of treatment. And there's just so many features that are negative in the methadone clinic system. We call it the Culture of Cruelty.
The cruelty is just stunning. The stories I've heard over the years never fail to astound me. The clinic is controlled by the Drug Enforcement Administration (DEA) and SAMHSA, the Substance Abuse and Mental Health Services Administration. The methadone clinic system was a compromise. It's like they really wanted abstinence, but know that methadone works, so they keep it locked inside a clinic system where people who take it are controlled and surveilled.
This system is ineffective. The retention rate in methadone clinics is below 50 percent. You can't get somewhere seven days a week on time, all the time. Due to the carceral setting, the humiliation and degradation, many people say fuck it! We're now in the third wave of the opioid overdose crisis where fentanyl is cheap and readily available. So it's easier to get fentanyl than it is to get methadone. Drug dealers will deliver fentanyl 24/7 right to your door in many places. No drug tests or counseling required and you can buy as much as you want. Methadone clinics can’t compete with that.
Moms for All Paths: There’s been a lot of fanfare about the new regulations. Can you tell us about that?
Helen Redmond:
The first thing I want to say is that SAMHSA is actually part of the problem.
The fact that SAMHSA is involved in any way in methadone is wrong. Why is a federal agency able to come between a healthcare provider and a patient in need of medication? This happens with no other medication, with the exception of buprenorphine.
SAMHSA works collaboratively with the DEA. For 40 years they have worked with the policing organization that is enforcing prohibition while being committed on paper to helping people with substance use and mental health issues. How can they do that when they’re working with the drug warriors in the DEA who are putting people in cages for using or dealing drugs?
SAMHSA has presided over the three waves of the opioid overdose crisis. We've lost up to a million people during those three waves. Year after year the rates of overdose deaths go up. It’s on SAMHSA’s watch. So on those grounds alone, they have no business being involved in methadone. The regulations hadn’t been updated for twenty years. Why? Why did it take so long? What were they doing during all that time that people have been dying from preventable overdose deaths? SAMHSA is a failed agency and needs to get the hell out of methadone prescribing along with the DEA. They all have blood on their hands.
Moms for All Paths: What are some of the changes in the new regulations?
Helen Redmond:
Probably the most important change for patients is the timetable for getting take-homes, doses you can take at home unsupervised, and not having to go to the clinic every single day. There are caveats which I'll get to, but for most patients the thing about the updated final rule that means the most is getting more take-homes more quickly. So now, the timetable is basically when you first start treatment the first one to 14 days, you can get up to a week's supply of take-home medication. From 15 to 30 days you can get 14 and then from 31 to 90 days in treatment, you can get up to 28 days. That sounds great, right? The less time you spend in these carceral settings, the better it is for your mental and physical health.
Another important change is the new guideline that counseling is optional, and that people cannot be dealt with punitively if they opt out.
Beyond that, I can't see much in this final rule that is really helpful to patients. The crucial thing to understand about the new regulations is that they are only guidelines. It is still up to each clinic to decide which rules they want to follow. They can still mandate counseling, or give patients fewer or no take-home bottles of methadone.
Clinic owners have embraced the new rules. The president of the American Association for the Treatment of Opioid Dependence, Mark Perrino, has said he’s grateful to SAMHSA for updating the rules. It tells you something that if the leadership of the trade association for opioid treatment prisons are on board with the new final rule you know that nothing fundamental is going to change. As I say in my article in Filter, the fox is still guarding the henhouse.
Moms for All Paths: Are there other reasons why the clinic owners might support the new rules?
Helen Redmond:
As I mentioned, a fatal flaw in the updated rules is that they are only guidelines, nothing is mandated or enforceable - the clinics still have the ability to do anything they want. So they love that. Another thing that people should know is that these regulations have the ability to get more people into methadone treatment, into liquid handcuffs. For example, now minors can get into treatment right away. Under the old rules, they had to fail two detox attempts first. Why they ever had that rule makes absolutely no sense, but the new guidelines eliminate it.
Interim treatment is when the clinic can offer methadone but not all the other services. The person can stabilize and not be at risk of overdose because they don't have to go to a poisoned street supply. And again, the clinics love this because it enrolls more patients and they make more profits.
The other thing that the clinics love about the SAMHSA Final Rule is they can induct people onto methadone using audio-visual means. And for some people who live far from a clinic, it's going to help them get into treatment quicker. But here’s the catch, they still have to come to the clinic to get the medication. And one more thing - methadone vans. Only OTPs can deploy them. There is no way they can scale up to deliver the medication to the vast amount of people who need it and they are a financial boondoggle. The vans are ridiculously expensive. I just wrote about methadone vans in New York City and just one costs over $500,000!
Moms for All Paths:
I wonder if the general public is not aware that the clinics are for-profit enterprises?
Helen Redmond:
According to a new report at STAT, nearly one-third of clinics are owned by private equity firms. There are seven methadone mega-chains. The more often people attend the clinic, the more money the clinic makes, so they have every incentive to keep people coming in, no matter how detrimental that is to the person’s life and functioning. If somebody gets 28 take-homes the clinic makes less money. Just do the math. That’s capitalism.
In addition to SAMHSA, each state has a State Opioid Treatment Authority and states often have more punitive and strict regulations than SAMHSA does. Together, federal, state and clinic regulations create a confusing situation. Which ones will be followed?
Moms for All Paths: What really doesn’t change with the new rules?
Helen Redmond:
The SAMHSA final rule does nothing to change this: Foundational to the methadone clinic system is the idea that the medication they dispense is a privilege, not a right. There is no other area of health care where we require patients to demonstrate, six or seven days a week, that they deserve their medicine. The massive power differential between patients and staff has not changed. The clinic still controls access to methadone.
And if you don't do what you're told, if you don't follow the rules and regulations, you won't get the medication you need to live. This power dynamic doesn’t exist with another medication. That is something that enrages me: The power that clinic staff have over patients to punish and control them. You are not free. Patients are still in liquid handcuffs with the new SAMHSA Final Rule.
Moms For All Paths: How has this illogical, damaging system evolved?
I think it has a lot to do with racism. Our country is based on racism, from health care to employment to education. Everything is stained by racism.
The clinic system was set up in the early 1960’s. And there was one study done by Dr. Robert Dupont in Washington, DC in a jail with mainly black men who were addicted to heroin. He said it showed if you give them methadone, it lowers the rate of crime. That’s debatable, actually. Nixon, a notorious racist, wanted to get re-elected and latched onto that. From the beginning, black people living in urban centers, crime, and drugs, were linked. No other medication has been tasked with reducing levels of crime, that speaks volumes about the origin of the methadone clinic system
So if people are going to get methadone, it's going to be in a system where they are controlled, monitored and punished because we view people who are addicted to opioids as criminals. We don't trust them so we're going to watch them take their methadone. We're going to force them to lift up their tongues and prove that they’ve swallowed the medication. We are going to watch them urinate during all those toxicology screenings. It’s infantilizing, degrading and humiliating!
Moms for All Paths: What about buprenorphine? Why is it so much easier to get than methadone, even though methadone is more effective for many people?
Helen Redmond:
Racism is foundational to the methadone clinic system. When buprenorphine, another synthetic opioid was approved by the FDA to treat opioid use disorder in 2000, it was targeted to white people in the suburbs. The people who were involved with getting that medication through the FDA said, “We don't want buprenorphine to be in a rigid clinic system like methadone. We want the medication to be prescribed by any doctor. So you go to an office, you get a prescription and you pick it up at the pharmacy, you get a 30 day supply.”
The racism was encoded, but buprenorphine was clearly marketed to white people who had suffered from the first wave of the opioid overdose crisis, prescription opioids like oxycontin and oxycodone. All of this is illustrated beautifully in the book WhiteOut: How Racial Capitalism Changed the Color of Opioids in America. And so buprenorphine is targeted to white people, and we know this because even today, the vast majority of people who take it are white. Studies show that Black people are not offered a prescription of buprenorphine as often as white people are. Methadone is for people of color and the poor and only available in an opioid treatment prison. Buprenorphine can be picked up at CVS. Now please don't get me wrong, I'm very happy that those white folks are getting buprenorphine. But I want everybody regardless of race or class to have access to this medication.
Moms for All Paths: Take-homes seem critical to a person on methadone getting their life together, with the ability to work at a job and take care of family and other responsibilities. Can you tell us more about how take-homes work now?
Helen Redmond:
There are five criteria that are used to determine if someone can have take-homes under the new rules. They will make it very difficult for the vast majority of patients to get take-homes.
A person can't be using other substances and get take-homes. So if you're using on top, if you're a recreational cocaine or meth user, alcohol, cannabis, as many of us are, you can’t get take-homes, even if you don’t have a problem with that substance.
You still have to have regular attendance at the clinic. It’s open to the clinic’s discretion to decide what is regular. You know, people miss dosing, not always their fault, right? I did a story recently where a woman who depends on transportation to her clinic which is an hour away. She is reliant on transportation provided by Medicaid, and they call her in the morning and say that they don’t have a driver. Or if the weather is bad, for example, a major snowstorm. So she misses a lot of doses and she can’t get take-homes.
An absence of serious behavioral problems that endanger the patient or the public and no recent history of diversion. Again, this is wide open to interpretation by clinic staff.
Medication can be safely transported and stored. When they talk about this, it is code for denying take-homes to people who are unhoused, sporadically unhoused, or housing insecure. This is where structural racism comes in. Who is disproportionately unhoused in this country? People of color.
Moms for All Paths: There has been a lot of talk about culture change in the methadone clinic system. Can you tell us what’s really going on with that?
Helen Redmond:
This is where SAMHSA, AATOD, and even some in the harm reduction community have selective amnesia. The culture we have now is a culture of cruelty of punishment. It is profoundly inhumane. We've got to be honest about that. We have to say that. So we've had this culture of cruelty for 50 years, where people have left treatment or been thrown out, and people are dying because of it. In current conversations, there is no recognition of that. There's this amnesia. People want to say that's in the past. It’s not in the past. It's very much with us today. Methadone clinics have blood on their hands.
They're saying, we have to create a new culture. And so what is this new culture that is created in clinics going forward? Here are the buzzwords they use: patient-centered care, shared decision making, we’re going to center everything around the patient. Do you really believe that the power differential will disappear? Do you really think that patients will be able to share decision making with the medical director or the nurse? It’s bullshit! Not going to happen.
Moms for All Paths: What do you think is the real solution to the problems presented by the methadone clinic system?
Helen Redmond:
The entire system needs to be abolished. Any healthcare provider should be able to write a prescription for methadone to treat opioid addiction. A patient should be able to go to the pharmacy of their choice and pick up a month’s supply just like every other medication in the pharmacopeia. Prescription parity. It's just common sense. We have to stop the siloing of methadone to treat addiction.
I don't believe you can reform the clinic system and there is no sense in trying when there is a much better, faster and humane way to get methadone to people. A rational system exists in Australia, Britain and New Zealand, where any doctor can prescribe methadone and patients can get it at the pharmacy.
That's what abolition does. It liberates everyone from opioid treatment prisons, they are a relic of the Nixonian era.
Moms for All Paths: What can we do to change the system?
Helen Redmond:
One of the problems that we face is that people who take methadone have not been able to organize effectively to fight for their rights. I’m thinking about back when AIDS patients first organized into ACT UP to fight for their right to medication, humane treatment and to end stigma. People who use methadone need to do that. So if moms have a loved one who is in the clinic system, can they become an advocate, form a union for patients?
I would also like to tell you about a piece of legislation that I oppose and would suggest that Moms oppose as well. It is called the Modernizing Opioid Treatment Access Act, (MOTAA) and it is sponsored by Representative Donald Norcross. I believe that this bill will set back our ability to free methadone from the methadone clinics if it’s passed, which I sincerely hope it is not. This bill only gives physicians certified in addiction medicine the right to prescribe methadone that is picked up at a pharmacy.
That sounds great, right?
The problem is that there are only about 6,000 board-certified addiction doctors and over 600,000 people who use methadone. This bill reinforces racial disparities in access to MOUD because who has access to specialists in this country? We know; white people who have commercial insurance or can pay out of pocket. How buprenorphine was made available is the cautionary tale. Medicaid is the largest payer at methadone clinics. Does every addiction specialist accept Medicaid? I think not. The vast majority of people who take methadone will remain trapped in the clinic system, in liquid handcuffs. I can’t support a bill that is racist and doesn’t help everyone.
We have to stop settling for incremental change. People have to stop saying MOTAA is a step in the right direction, because it’s not! We need to abolish the racist and inhumane methadone clinic system completely and transition to a pharmacy-based dispensing system. That is what will liberate everyone and it’s the only way to end the opioid overdose crisis.
Moms for All Paths: Thank you so much for your time and this valuable information! Where can we find more information?
Helen Redmond:
Here is a link to a webinar that gives more information about the new SAMHSA Final Rule. Here are some articles in Filter that address the problems in the methadone clinic system:
With New Final Rule, SAMHSA Isn’t Coming To Save Us
Daily Methadone Dosing Creates Rural Transportation Nightmare
Rep. Norcross Admits His Bill Isn’t Enough. We Should Too.
https://filtermag.org/whiteout-opioids-race-capitalism/
Moms for All Paths: Thank you so much for your time and the essential, life-saving work you are doing!
Don’t forget to follow us on Twitter, now X, at @MomsAllPaths
And if you’re not already a member, join the Facebook group at https://www.facebook.com/groups/momsforallpath



Thank you for sharing this important information about how methadone treatment is being provided to those with SUD. Limiting this life saving medication through an ineffective clinic system is causing so much harm and suffering. Liberate the methadone !